Uterine Fibroid Embolization
Guide to Uterine Fibroid Embolization
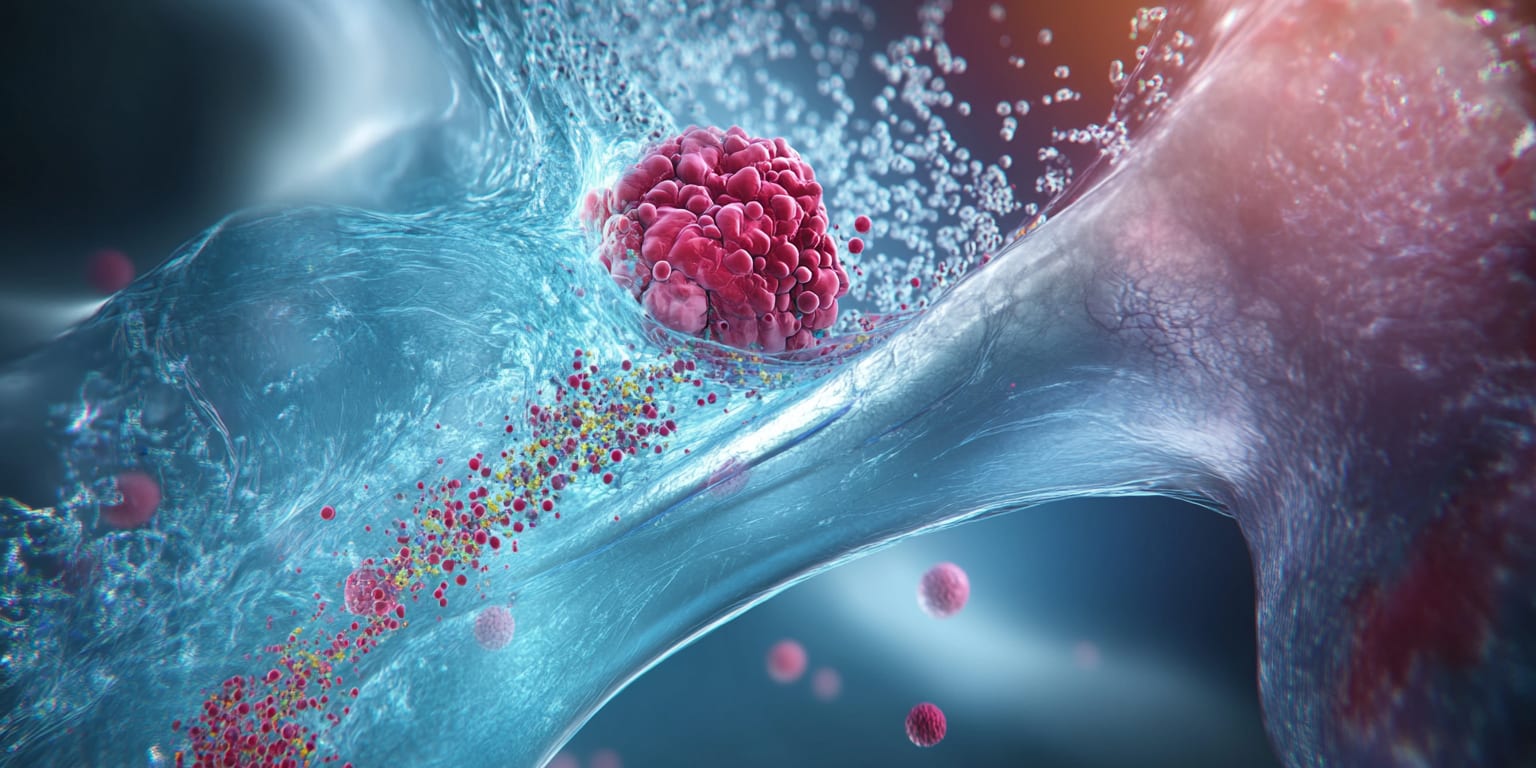
Uterine Fibroid Embolization (UFE) is a minimally invasive image-guided procedure used to treat uterine fibroids by blocking their blood supply and causing them to shrink.
What is Uterine Fibroid Embolization?
Uterine Fibroid Embolization (UFE), sometimes called Uterine Artery Embolization (UAE), is a minimally invasive, image-guided procedure that shrinks uterine fibroids—the benign tumors that develop in the muscular wall of the uterus. An interventional radiologist inserts a catheter through a small incision in the wrist or groin and navigates to the uterine arteries, where microscopic particles are released to block blood flow to the fibroids. Without a blood supply, the fibroids shrink and symptoms gradually improve.
Why is the Procedure Performed?
UFE is performed to alleviate symptoms caused by uterine fibroids, including:
- Heavy or prolonged menstrual bleeding that can lead to anemia.
- Pelvic pain or pressure.
- Frequent urination or constipation due to fibroid pressure on adjacent organs.
- Abdominal bloating or an enlarged uterus.
- Pain during intercourse.
The procedure offers an alternative to surgical options such as hysterectomy (removal of the uterus) and myomectomy (surgical removal of fibroids), preserving the uterus and offering quicker recovery.
How is the Procedure Performed?
UFE is conducted in an angiography suite under conscious sedation and local anesthesia.
- Vascular Access: A tiny incision is made in the groin (common femoral artery) or wrist (radial artery). A catheter is introduced into the artery.
- Navigation: Using real-time fluoroscopic imaging, the catheter is advanced into the uterine arteries.
- Embolization: A contrast dye identifies blood flow, then biocompatible microspheres are slowly injected to block arterial branches feeding the fibroids while preserving the main uterine blood supply.
- Completion: Once adequate embolization is confirmed, the catheter is removed, and manual pressure or a closure device is applied to the incision site.
The procedure typically lasts 60–90 minutes. Most patients stay for a short observation period and are discharged the same day or after an overnight stay, depending on clinical judgment.
What are the Risks and Benefits of the Procedure?
- Benefits:
- Relief from heavy bleeding, pelvic pain, and pressure symptoms.
- Minimally invasive—no large incisions or uterine removal.
- Outpatient or short hospital stay with rapid recovery (about 1–2 weeks).
- High success rate (85–90%) with sustained symptom control.
- Risks:
- Post-embolization syndrome (temporary pain, low-grade fever, malaise).
- Infection of the uterus or puncture site.
- Allergic reaction to contrast dye.
- Non-target embolization that can damage healthy tissue.
- Premature ovarian failure or early menopause (rare, higher risk if >45 years old).
- Need for additional treatment or surgery if symptoms persist.
Discuss these risks and benefits with your physician to decide if UFE is appropriate for you.
Preparing for Uterine Fibroid Embolization
What to Expect During the Procedure
During UFE, you will remain awake but relaxed under conscious sedation. The access site will be numbed, so you should feel only slight pressure. You may experience a warm sensation when contrast dye is injected. The procedure typically lasts about 60–90 minutes.
Pre-op Instructions
- Fasting: Do not eat or drink anything for 6–8 hours before the procedure.
- Medication Review: Inform your physician of all medications, supplements, and allergies. You may need to adjust or temporarily discontinue certain drugs.
- Pre-Procedure Tests: Blood tests and imaging studies (ultrasound or MRI) may be performed to evaluate fibroid size, number, and location.
- Transportation: Arrange for a responsible adult to drive you home.
Medications to Avoid Before the Procedure
- Blood Thinners: Anticoagulants and antiplatelet agents (e.g., warfarin, clopidogrel, aspirin) may need to be stopped several days prior, as directed by your physician.
- NSAIDs: Non-steroidal anti-inflammatory drugs might be paused to minimize bleeding risk.
- Herbal Supplements: Garlic, ginkgo, ginseng, and others can increase bleeding risk and should be discontinued.
- Diabetes Medications: You may need to adjust insulin or oral hypoglycemics due to fasting; follow your physician's guidance.
What to Bring to the Surgery Center
- Medication List: Include all prescription and over-the-counter medications and dosages.
- Personal Identification and Insurance Information.
- Comfort Items: Loose-fitting clothes and personal hygiene items for an overnight stay if advised.
What to Expect After the Procedure
- Immediate Recovery: You will rest in a recovery area where vital signs and the access site are monitored. Pain medication and anti-nausea drugs are provided as needed.
- Observation: Most patients are observed for 4–6 hours before discharge. Some may stay overnight for pain control.
Post-op Instructions
- Activity: Limit strenuous activity and heavy lifting for 7 days. Light walking is encouraged.
- Access Site Care: Keep the bandage clean and dry. Follow instructions on showering and dressing changes.
- Hydration: Drink plenty of fluids to help flush contrast dye.
- Medication: Take prescribed pain relievers and antibiotics (if given) exactly as directed. Resume other medications per your physician's advice.
Recovery Tips
- Rest: Plan for a few days of rest at home.
- Manage Pain: Use prescribed pain medication or over-the-counter NSAIDs as directed.
- Heat Therapy: A heating pad can help relieve cramping.
- Balanced Diet: Prioritize iron-rich foods if you experienced heavy bleeding and maintain a fiber-rich diet to prevent constipation from pain medications.
When to Seek Medical Attention
- Emergency Symptoms: Severe pelvic pain not relieved by medication, heavy vaginal bleeding, persistent high fever (>101°F), foul-smelling discharge, or signs of infection at the access site.
- Unusual Concerns: Contact your physician if you experience worsening symptoms or have concerns about recovery.
By understanding what to expect before, during, and after Uterine Fibroid Embolization, you can help ensure a smoother procedure and recovery. Always follow your healthcare provider's instructions and communicate any concerns promptly.
