Kyphoplasty
Guide to Kyphoplasty
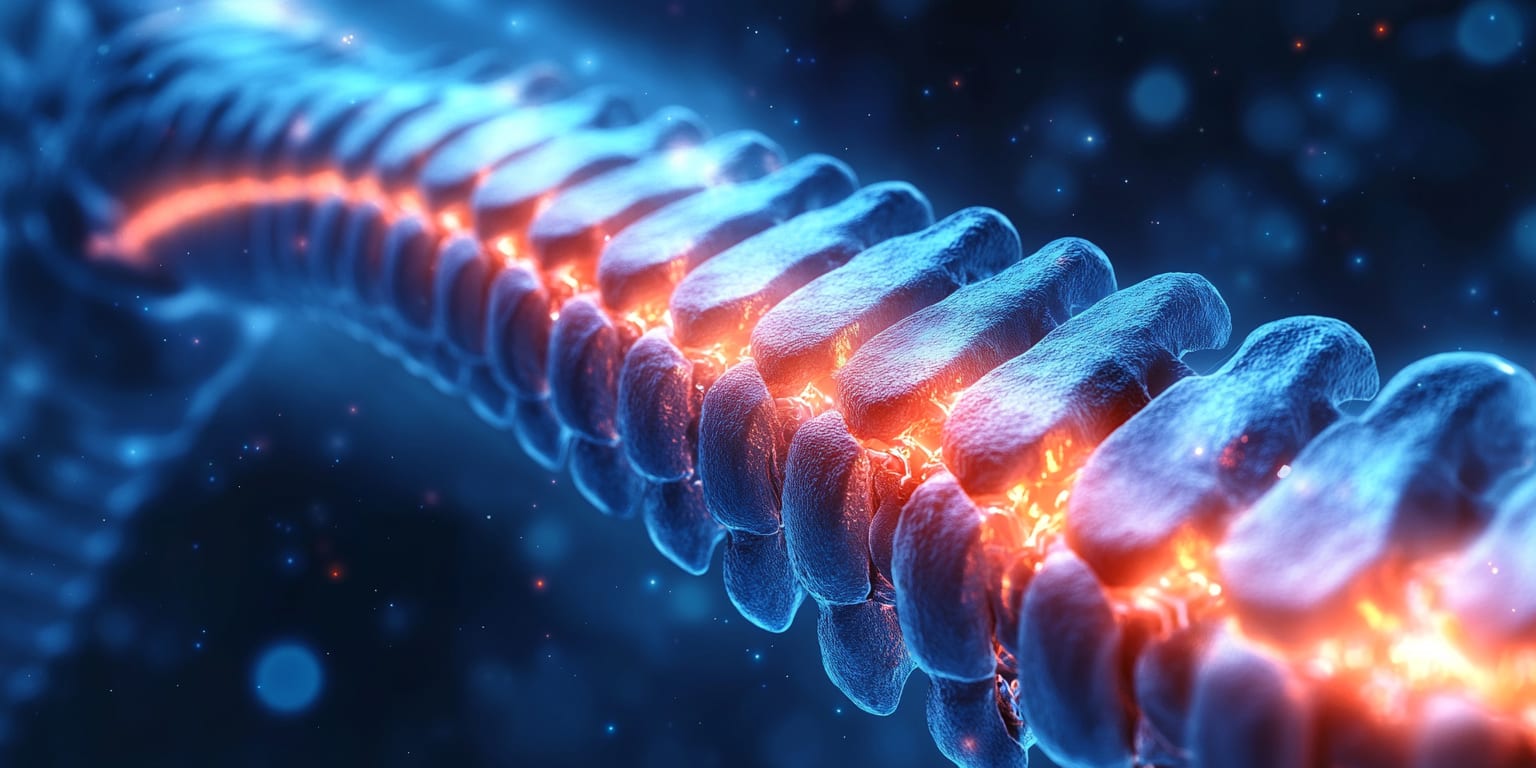
Kyphoplasty is a minimally invasive procedure that stabilizes spinal compression fractures and restores vertebral height by injecting bone cement after balloon expansion.
What is Kyphoplasty?
Kyphoplasty is a minimally invasive spine procedure designed to treat painful vertebral compression fractures (VCFs). An interventional radiologist or spine specialist inserts a narrow tube into the collapsed vertebra, inflates a balloon to create a cavity and partially restore height, then fills the space with fast-hardening bone cement (polymethylmethacrylate). The cement stabilizes the fracture, alleviates pain, and can improve posture by reducing spinal curvature (kyphosis).
Why is the Procedure Performed?
Kyphoplasty is recommended to:
- Relieve back pain caused by osteoporotic or cancer-related vertebral compression fractures.
- Stabilize the fractured vertebral body to prevent further collapse.
- Improve mobility, quality of life, and reduce reliance on pain medication.
- Restore some lost vertebral height and correct spinal alignment, decreasing kyphosis.
How is the Procedure Performed?
Kyphoplasty is performed under fluoroscopic or CT guidance in a sterile procedure suite:
- Patient Position: You lie face-down on a padded table; vital signs are monitored.
- Local Anesthesia & Sedation: The skin and muscles over the affected vertebra are numbed; IV sedation keeps you relaxed and comfortable.
- Access: A small incision is made, and a trocar (hollow needle) is advanced into the fractured vertebral body.
- Balloon Inflation: A deflated orthopedic balloon is inserted through the trocar and gently inflated to create a cavity and elevate the collapsed bone.
- Cement Injection: After removing the balloon, viscous bone cement is injected under low pressure, filling the cavity and hardening within minutes.
- Closure & Recovery: The instruments are removed, a sterile dressing is applied, and you are moved to recovery for observation.
The procedure typically lasts 30–45 minutes per vertebra.
What are the Risks and Benefits of the Procedure?
- Benefits:
- Rapid and significant pain relief.
- Stabilization of the fractured vertebra.
- Potential restoration of vertebral height, reducing spinal deformity.
- Quick recovery with minimal hospital stay.
- Risks:
- Leakage of cement into nearby veins or soft tissue.
- New fractures in adjacent vertebrae.
- Infection, bleeding, or allergic reaction to materials.
- Anesthesia-related complications.
Discuss with your physician how these risks apply to your specific medical condition.
Preparing for Kyphoplasty
What to Expect During the Procedure
You will be awake but sedated. You may feel pressure but should not experience sharp pain. The procedure is short, and many patients notice pain relief immediately or within a day.
Pre-op Instructions
- Fasting: Do not eat or drink for 6–8 hours before your appointment.
- Medication Review: Provide a complete list of medications, especially blood thinners or osteoporosis drugs. Some may need adjustment.
- Imaging: Recent MRI or CT scans help confirm fracture age and suitability for Kyphoplasty.
- Transportation: Arrange for someone to drive you home.
Medications to Avoid Before the Procedure
- Blood Thinners: Anticoagulants (warfarin, apixaban) and antiplatelets (clopidogrel, aspirin) may require temporary discontinuation.
- NSAIDs: May be paused per physician guidance.
- Herbal Supplements: Ginkgo, garlic, and others that affect bleeding should be stopped.
- Diabetes Medications: Adjust as instructed due to fasting.
What to Bring to the Surgery Center
- Medication List with dosages.
- Photo ID and Insurance Card.
- Comfortable Clothing and slip-on shoes for discharge.
What to Expect After the Procedure
- Immediate Recovery: You will lie flat for about an hour while the cement cures. Vital signs and neurological status are monitored.
- Mobility: Most patients stand and walk with reduced pain before discharge.
- Diet: Light food and fluids are allowed once fully awake.
Post-op Instructions
- Activity: Resume light activities as tolerated; avoid heavy lifting and high-impact exercise for 4–6 weeks.
- Wound Care: Keep the small bandage clean and dry for 24 hours.
- Medications: Take prescribed pain relievers as needed; resume other medications per your doctor's advice.
- Bone Health: Continue or begin osteoporosis treatment (calcium, vitamin D, bisphosphonates) as directed.
Recovery Tips
- Gradual Exercise: Engage in low-impact activities like walking to rebuild strength.
- Posture: Practice good body mechanics and consider physical therapy.
- Lifestyle: Maintain a calcium-rich diet, avoid smoking, and limit alcohol to support bone health.
When to Seek Medical Attention
- Emergency Symptoms: Sudden severe back pain, leg weakness or numbness, loss of bowel or bladder control, fever, or drainage from the incision site.
- Persistent Issues: Contact your physician if pain does not improve or new symptoms develop.
By understanding what to expect before, during, and after Kyphoplasty, you can help ensure a smooth procedure and recovery. Always follow your healthcare provider's instructions and communicate any concerns promptly.
Frequently Asked Questions
Hemorrhoidal Artery Embolization
Hemorrhoidal Artery Embolization (HAE) is a minimally invasive image-guided procedure that treats symptomatic hemorrhoids by blocking the arteries that supply blood to the hemorrhoidal cushions.
Prostate Artery Embolization
Prostate Artery Embolization (PAE) is a minimally invasive image-guided procedure that reduces urinary symptoms caused by benign prostatic hyperplasia (BPH) by blocking blood flow to the enlarged prostate.
