Dialysis Access Management
Guide to Dialysis Access Management
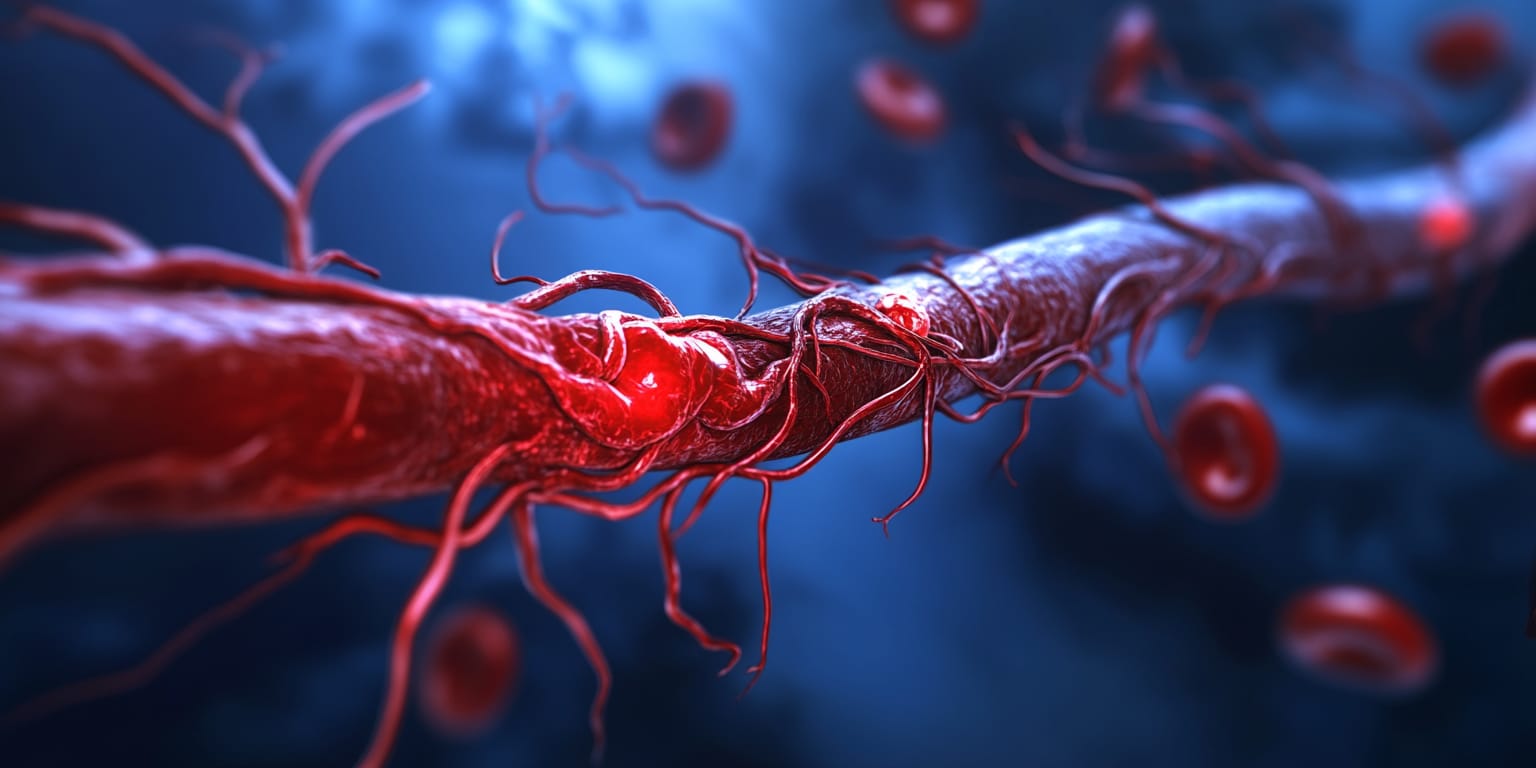
Dialysis Access Management encompasses minimally invasive procedures to create, maintain, and restore function to arteriovenous fistulas (AVF) and grafts used for hemodialysis.
What is Dialysis Access Management?
Dialysis Access Management includes a spectrum of image-guided procedures aimed at establishing and preserving reliable vascular access for hemodialysis. Interventional radiologists use minimally invasive techniques—such as angioplasty, thrombolysis, mechanical thrombectomy, ultrasound-guided fistula creation, and stent or catheter placement—to optimize blood flow through arteriovenous fistulas (AVF), grafts, or central venous catheters.
Why is the Procedure Performed?
A functioning access site is critical for patients with end-stage renal disease (ESRD) receiving life-sustaining hemodialysis. Common reasons for intervention include:
- Stenosis causing decreased blood flow and inadequate dialysis.
- Acute thrombosis (clot) leading to access failure.
- Prolonged bleeding, aneurysm, or high venous pressures.
- Malfunctioning tunneled catheters or need for new catheter placement.
- Maturation assistance for newly created fistulas.
Prompt treatment restores access patency, prevents catheter dependence, and reduces infection risk.
How is the Procedure Performed?
Procedures are performed in an outpatient vascular suite under ultrasound and fluoroscopic guidance:
- Assessment: Fistulogram or angiogram maps the access and identifies problems.
- Angioplasty: A balloon catheter is inflated at stenotic segments to widen the vessel.
- Stent Placement: If recoil or elastic narrowing persists, a stent is deployed.
- Thrombectomy/Thrombolysis: Mechanical devices and/or clot-dissolving medications clear blockages, restoring flow.
- Catheter Work: Exchange, reposition, or removal of tunneled dialysis catheters when indicated.
- Hemostasis: Access sites are closed with manual pressure or a closure device.
Most procedures last 30–60 minutes. Patients are observed for 1–2 hours before discharge.
What are the Risks and Benefits of the Procedure?
- Benefits:
- Restores or maintains adequate blood flow, ensuring effective dialysis.
- Minimally invasive with rapid recovery.
- Reduces need for surgical revision and central catheter placement.
- Improves quality of life by minimizing missed dialysis sessions.
- Risks:
- Bleeding or hematoma at the puncture site.
- Vessel perforation or dissection (rare, usually treated immediately).
- Infection or allergic reaction to contrast dye.
- Restenosis or re-thrombosis requiring repeat intervention.
Discuss individual risk factors with your physician.
Preparing for Dialysis Access Management
What to Expect During the Procedure
You will lie on an X-ray table. The access arm or catheter site is cleaned and numbed. Mild IV sedation keeps you relaxed. You may feel pressure but should not experience significant pain.
Pre-op Instructions
- Fasting: Do not eat solid food for 4–6 hours prior; clear liquids are usually allowed.
- Medication Review: Continue most medications; blood thinners may be adjusted per physician advice.
- Dialysis Schedule: Coordinate timing so the intervention occurs shortly after a dialysis session when possible.
- Transportation: Arrange a ride home; driving is not recommended post-sedation.
Medications to Avoid Before the Procedure
- Anticoagulants/Antiplatelets: Warfarin, apixaban, clopidogrel, or aspirin doses may be modified—follow instructions.
- NSAIDs: May be limited to reduce bleeding risk.
- Herbal Supplements: Stop ginkgo, garlic, or ginseng 5–7 days prior.
What to Bring to the Surgery Center
- Access arm exposed: Wear loose clothing allowing easy access to fistula/graft.
- Medical Information: Medication list, dialysis schedule, ID, and insurance card.
What to Expect After the Procedure
- Observation: Staff monitor your vitals and access site; you can eat and drink when fully awake.
- Thrill Check: Your nurse will confirm the vibration (thrill) over the fistula has returned.
- Discharge: Most patients leave within 1–2 hours.
Post-op Instructions
- Activity: Avoid heavy lifting with the access arm for 24 hours.
- Site Care: Keep bandage dry for 12–24 hours; monitor for bleeding or swelling.
- Dialysis: Resume as scheduled unless told otherwise.
- Hydration: Drink fluids unless on fluid restriction from dialysis team.
Recovery Tips
- Monitor Access: Check thrill daily and report changes.
- Arm Care: Avoid tight clothing, blood pressure cuffs, or venipuncture on the access arm.
- Healthy Lifestyle: Diet and fluid management per renal team guidance.
When to Seek Medical Attention
- Emergency Symptoms: Sudden loss of thrill, swelling, prolonged bleeding (>20 minutes), fever, or severe arm pain.
- Persistent Issues: Contact your physician if redness, drainage, or access dysfunction recurs.
By understanding the importance of Dialysis Access Management and following your care team's instructions, you can help maintain a reliable lifeline for effective hemodialysis and better health outcomes.
Frequently Asked Questions
Peripheral Artery & Vein Intervention
Peripheral Artery & Vein Interventions improve blood flow within the arms and legs to remove blood clots, and decrease pain or swelling of the extremity.
Genicular Artery Embolization
Genicular Artery Embolization (GAE) is a minimally invasive image-guided procedure that treats chronic knee pain from osteoarthritis by reducing abnormal blood flow to the knee's inflamed lining.
