Hemorrhoidal Artery Embolization
Guide to Hemorrhoidal Artery Embolization
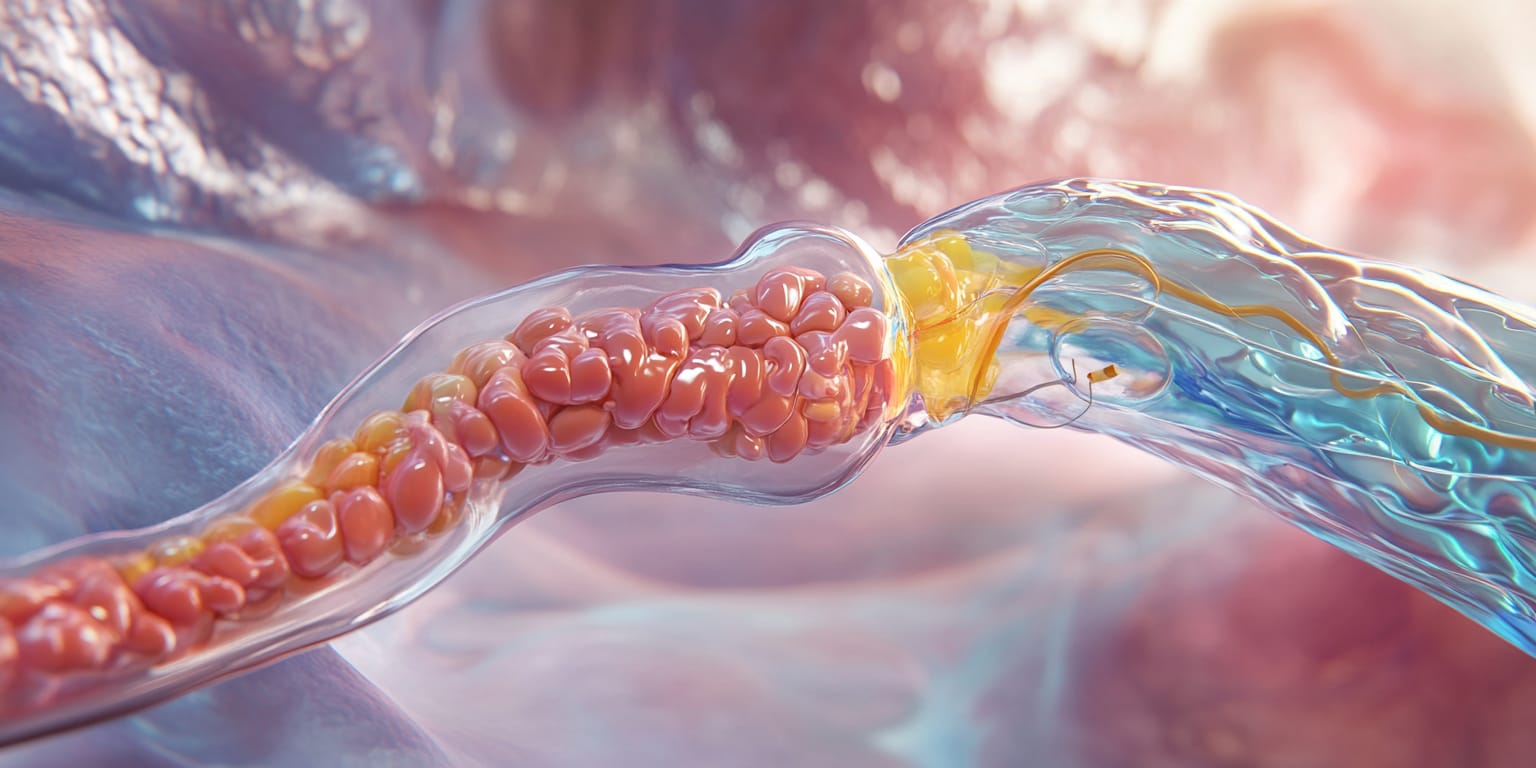
Hemorrhoidal Artery Embolization (HAE) is a minimally invasive image-guided procedure that treats symptomatic hemorrhoids by blocking the arteries that supply blood to the hemorrhoidal cushions.
What is Hemorrhoidal Artery Embolization?
Hemorrhoidal Artery Embolization (also called Emborrhoid) is a minimally invasive treatment for internal hemorrhoids that uses X-ray guidance to block the superior rectal (hemorrhoidal) arteries feeding the swollen vascular cushions. An interventional radiologist advances a catheter through the arteries and releases microscopic particles that reduce blood flow, causing hemorrhoids to shrink and symptoms such as bleeding, itching, and pain to resolve—without surgical excision of tissue.
Why is the Procedure Performed?
HAE is performed to manage symptomatic hemorrhoids when conservative therapies have failed or surgery is not desired. Indications include:
- Recurrent rectal bleeding leading to anemia.
- Pain, itching, or discomfort during bowel movements.
- Prolapse of internal hemorrhoids (grade II–III).
- Contraindication to or refusal of surgical hemorrhoidectomy.
How is the Procedure Performed?
The procedure is conducted in an angiography suite under conscious sedation and local anesthesia.
- Vascular Access: A small incision is made in the wrist (radial artery) or groin (femoral artery). A thin catheter is inserted into the arterial system.
- Navigation: Using fluoroscopy, the catheter is advanced into the inferior mesenteric artery and then into the superior rectal arteries supplying the hemorrhoids.
- Embolization: After contrast dye identifies the branches, calibrated particles (100–300 µm) are slowly injected until blood flow to the hemorrhoids is reduced.
- Completion: Final imaging confirms successful embolization. The catheter is removed, and pressure or a closure device is applied to the access site.
The procedure lasts 30–60 minutes, and patients are typically discharged the same day.
What are the Risks and Benefits of the Procedure?
- Benefits:
- Significant reduction or cessation of rectal bleeding.
- Rapid recovery with minimal post-procedural pain.
- Preserves anal sphincter integrity—no risk of incontinence.
- Outpatient procedure with no general anesthesia.
- Risks:
- Bruising or hematoma at the access site.
- Mild pelvic or rectal discomfort (post-embolization syndrome).
- Transient diarrhea or constipation.
- Non-target embolization leading to rectal or bladder ischemia (rare).
- Infection or allergic reaction to contrast dye (rare).
Discuss these benefits and risks with your physician to decide if HAE is right for you.
Preparing for Hemorrhoidal Artery Embolization
What to Expect During the Procedure
You will be awake but relaxed under conscious sedation. The access site will be numbed, so you should only feel minimal pressure. The procedure generally takes under one hour.
Pre-op Instructions
- Fasting: Do not eat or drink for 6–8 hours before the procedure.
- Bowel Prep: In some cases, a mild enema or laxative may be prescribed the night before to clear the rectum.
- Medication Review: Provide a list of all medications, supplements, and allergies. Certain drugs may need to be halted temporarily.
- Transportation: Arrange for a responsible adult to drive you home.
Medications to Avoid Before the Procedure
- Blood Thinners: Anticoagulants and antiplatelets (warfarin, apixaban, clopidogrel, aspirin) may need to be paused per physician guidance.
- NSAIDs: Could be stopped to minimize bleeding risk unless needed for pain.
- Herbal Supplements: Discontinue ginkgo, garlic, ginseng, or others that affect clotting.
- Diabetes Medications: Adjust insulin or oral agents as directed due to fasting.
What to Bring to the Surgery Center
- Medication List with dosages.
- Photo ID and Insurance Information.
- Comfortable Loose-Fitting Clothing.
What to Expect After the Procedure
- Immediate Recovery: You will rest while your vital signs and access site are monitored. Mild pelvic discomfort is managed with medication.
- Diet: Light meals are usually tolerated soon after the procedure. Drink ample fluids to help flush contrast dye.
- Discharge: Most patients leave after 2–3 hours of observation.
Post-op Instructions
- Activity: Avoid strenuous exercise and heavy lifting for 48 hours. Gentle walking is encouraged.
- Access Site Care: Keep the bandage dry for 24 hours, then follow instructions for showering and dressing changes.
- Bowel Habits: Maintain a high-fiber diet and adequate hydration to prevent constipation. Over-the-counter stool softeners can help.
- Medications: Take prescribed pain relievers and resume regular medications per your doctor's advice.
Recovery Tips
- Fiber & Fluids: A diet rich in whole grains, fruits, and vegetables promotes soft stools.
- Avoid Straining: Do not sit on the toilet for prolonged periods; consider a footstool to improve posture.
- Warm Sitz Baths: Short warm baths can soothe the anal area during healing.
When to Seek Medical Attention
- Emergency Symptoms: Severe rectal pain, profuse bleeding, fever >101°F, difficulty urinating, or signs of infection at the access site.
- Persistent Issues: Contact your physician if bleeding persists beyond a few weeks or if discomfort worsens.
By understanding what to expect before, during, and after Hemorrhoidal Artery Embolization, you can help ensure a smoother procedure and recovery. Always follow your healthcare provider's instructions and report any concerns promptly.
Frequently Asked Questions
Genicular Artery Embolization
Genicular Artery Embolization (GAE) is a minimally invasive image-guided procedure that treats chronic knee pain from osteoarthritis by reducing abnormal blood flow to the knee's inflamed lining.
Kyphoplasty
Kyphoplasty is a minimally invasive procedure that stabilizes spinal compression fractures and restores vertebral height by injecting bone cement after balloon expansion.
